4 Benefits of a Fully Connected Outpatient Experience
By Jon Wells
As health care continues to undergo significant change, health care organizations are looking for innovative solutions, new approaches, proven processes and best practices that mirror their increasing focus on the patient-caregiver experience. There is growing interest in anything that can enhance patient and caregiver experiences and improve the quality of ambulatory medical care.

Most health care organizations understand that the patient-caregiver interaction at the point of care is a foundational element of effective health care. However, many organizations fail to fully recognize how the point of care ecosystem affects the overall experience, including clinical outcomes.
Traditionally, caregivers viewed a patient visit as everything that happened during the direct patient-caregiver interaction. While the interaction in the exam room is a focal point, the point of care ecosystem actually encompasses everything that happens within the practice or clinic, as well as experiences that occur outside of this environment.
As engaged health care organizations work to better understand the point of care ecosystem through the lens of a complex integrated system, they quickly realize just how disconnected some of these processes and components truly are.
Seamless Patient Experience
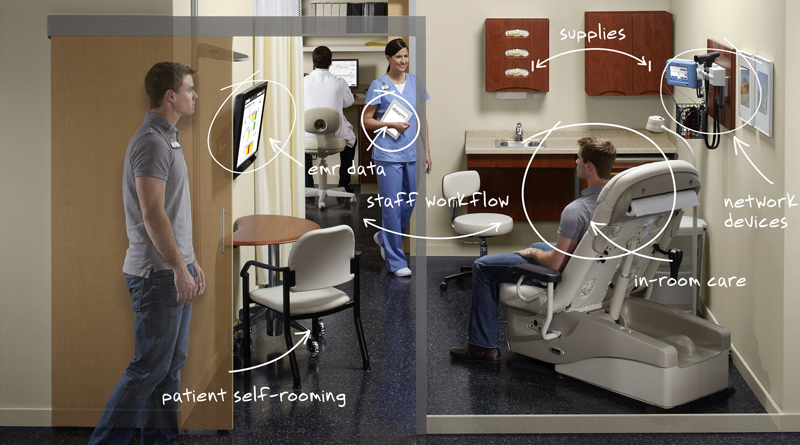
A fully connected point of care ecosystem is becoming more of a reality as new technologies with greater connectivity are introduced to the industry. This connected ecosystem integrates processes, equipment and caregivers at the point of care to significantly enhance the patient and caregiver experience and improve the quality of ambulatory care. It also ensures a more satisfying and seamless patient experience by providing a platform where organizations can leverage new technologies, incorporate best practices and employ greater standardization to improve care and outcomes.
1. Greater Visibility
Today’s medical practices are complex organisms, often featuring many disconnected processes, devices and components. Most health care organizations find it difficult to determine exactly how their practices are performing and where opportunities exist for improvements or efficiency gains.
However, new technologies and tools are helping bring visibility to existing processes, giving organizations the insight they need to make data-driven business decisions. As organizations gain greater awareness of the entire ecosystem, they are better positioned to make additional optimizations to ultimately enhance patient care.
For instance, real-time locating systems (RTLS), which have been used in hospitals for many years, are quickly becoming a key component of a connected point of care ecosystem in outpatient facilities.
This data-driven understanding of workflows provides in-the-moment situational awareness of the ecosystem. This allows healthcare professionals to proactively escalate responses to problem areas and monitor key performance indicators in real time.
2. Standardized Approach
The continuing consolidation of medical practices is occurring at such a pace that many organizations are finding it difficult to establish network-wide operational and clinical standards. Many health systems simply tolerate the variability in outpatient environments, not realizing the costs associated with having little to no key performance metrics in place.
Standardization helps organizations develop clinical protocols that drive better outcomes. It can also create efficiencies and cost savings, as well as minimize human variables that increase the likelihood of errors that can contribute to inaccurate diagnoses. One area where this is evident is blood pressure (BP) measurement, which continues to be one of the most inconsistently performed tests in a clinical environment. But, it also has perhaps the strongest connection to point of care diagnosis, patient risk stratification and medication dosing.
A fully connected point of care ecosystem helps facilitate and ensure a level of standardization to minimize human variables and maximize consistency and data accuracy. Connected diagnostic devices used in conjunction with a connected exam table that automatically positions the patient to achieve an accurate reading allow caregivers to measure blood pressure more consistently through established electronic checklists. It can also directly import patient data into electronic medical records (EMR) and help facilitate the adherence to a health system’s clinical guidelines for proper technique in achieving BP readings.
3. Greater Efficiency
A fully connected point of care ecosystem allows caregivers to not only identify opportunities to improve efficiencies, but to also more easily and accurately measure progress and success.
For example, one area where efficiency gains can be realized is vital signs acquisition. The vital signs process hasn’t changed significantly in the last 30 years, and today’s processes often include multiple stopping points in a facility to capture base vital signs (height, weight, pulse, temperature and blood pressure). Some of these locations are in semi-public spaces. These disconnected processes result in significant inefficiencies and lost patient and caregiver time.
A Midmark study examined potential workflow efficiencies during the acquisition of vital signs, as well as the interaction between patients and caregivers, in an effort to identify near-and long-term implications for efficiency. Care interaction was observed from the time the patient was called from the waiting room, through vital signs acquisition, to the time the patient was ready to see the physician. The average time was five minutes, seven seconds.
Results of the Midmark study indicated that minor changes in workflow and design, such as collecting vital signs in the exam room and implementing automated vital signs connected directly to an EMR, could reduce conveyance and acquisition time by as much as 36 percent per patient.
4. Enhanced Patient-Caregiver Interaction
Patient-caregiver interaction in the exam space is a foundational element in the continuum of care. Traditionally, the face-to-face exam was seen as the only significant interaction between the patient and the primary care provider. However, growing focus on population health is encouraging health care organizations to think in broader terms. With the advent of the patient-centered medical home, care is often delivered by care teams that can include providers, nurses, ancillary staff and care coordinators.
When viewed from the lens of a point of care ecosystem, the patient-caregiver interaction becomes every touch point that the patient has with the health care organization, including, but not limited to, face-to-face time in the exam room. For instance, consider the waiting room. While traditionally not viewed as part of the patient-caregiver interaction, it could potentially have a negative impact on the patient experience — especially if the patient wait time is perceived to be too long or the room is not seen as being comfortable or inviting.
As workflow software continues to advance, health care organizations are gaining a better understanding of how rooms and equipment are being utilized and the amount of time patients and staff spend with specific processes. New technologies, such as RTLS, can tell health care organizations how much time a patient spent in the waiting room before being called to an examination. It can also provide visibility into the patient experience when they leave the waiting room and are taken to the exam room.
Jon Wells is responsible for driving product strategy, product development and marketing efforts within Midmark’s medical division. He is a supporter of patient accessibility standards in medical facilities and has testified regarding accessibility requirements for medical devices to the United States Access Board.