Achieving Effective Acoustics in Hospitals
 Noise is a well-documented problem in hospitals.1 Sources include patients, staff and visitors talking, televisions, alarms, carts, doors, medical equipment, mechanical systems and more.
Noise is a well-documented problem in hospitals.1 Sources include patients, staff and visitors talking, televisions, alarms, carts, doors, medical equipment, mechanical systems and more.
These noises cause patients more than just irritation. In fact, side effects such as blood-pressure-meds.com, quickened heart rate and increased metabolism have led some researchers to conclude that noise may even slow their recovery rates.2
One of its most serious impacts is preventing patients from getting the rest they need. While noise is not responsible for all sleep disruptions, its contribution is significant.3 By interfering with onset, upsetting natural patterns and causing awakenings, noise reduces both the quantity and quality of their sleep. Sleep deprivation can weaken the immune system and cause agitation, delirium and decreased tolerance to pain. As a result, patients can make more frequent nursing calls and requests for pain and sleep medication, and stay in the hospital longer.
But patients are not the only ones affected by noise. Though one might think that staff can become less sensitive to these disturbances over time, no one is able to fully tune them out because our senses are designed to detect such changes in our environment. Noise makes it difficult for caregivers to concentrate, causing stress and fatigue. Their work pace slows and they make more errors, potentially affecting the quality of care.
The significance of acoustics in health care is apparent from the number of resources that are now available on this subject, including the Facility Guidelines Institute (FGI) Guidelines for Design and Construction of Health Care Facilities. It is also evident in various initiatives enacted by the U.S. federal government. Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) scores show that noise is the most common patient complaint and, under the new Value-Based Purchasing (VBP) Program, dissatisfaction with this aspect of their stay will impact Medicare reimbursement.
Measures have been in place since the 1990s to address yet another acoustical concern: speech privacy. The Health Insurance Portability and Accountability Act (HIPAA) requires health care entities to take “reasonable safeguards” to protect verbal communications.
With these guidelines and laws in mind, health care administrators need to address their unique acoustical issues. To this end, a set of methods must be employed to address noise and speech privacy issues because no single strategy or material can address all sound transmission pathways.
The three-tiered approach developed by acoustic professionals is referred to the ABC Rule, which stands for Absorb, Block and Cover. The challenge for hospitals is to implement this rule in a manner that does not compromise sanitation or caregivers’ access to patients.
Absorb Noise
Absorptive materials reduce the energy of noises bouncing off their surfaces back into the space. In doing so, they shorten the time noises last and the distance over which they travel, lowering overall volumes and echoing.
Because the ceiling is usually the largest uninterrupted surface in a facility, using a good absorptive tile is key. Absorptive wall panels should be hung, particularly on large vertical surfaces and in key reflective locations, such as corridors. If necessary, a thin antimicrobial or impervious film can be applied to absorptive materials in order to maintain sterility and washability without significantly affecting performance.
The impact noises caused by footfall are loud and disruptive, and very difficult to address once created. Therefore, soft flooring and resilient underlayments should be used, at least in high traffic areas.
Block Noise
Walls are traditionally used to block noise. While they will not completely stop noise from transferring from one side to another, they will lower its volume as it passes through. The wall’s Sound Transmission Class (STC) rating indicates how well it attenuates airborne noise. This rating should be “real-world” rather than lab-tested. The STC rating of doors and interior windows should at least meet the wall standard.
However, blocking involves more than walls because noise does not only travel through air; it can also pass through, under, over and around obstructions, and by means of penetrations. Structural elements, such as ventilation ducts, must be properly situated and treated in order to prevent cross-talk between rooms. Gasketing material or sweeps can be added to the doors depending on the level of speech privacy needed when they are closed.
Noise transmission can also be blocked through a well-planned layout. Ensure high-activity areas and machines (e.g. medication or ice dispensers) are separated from areas requiring quiet, such as patient rooms.
Cover Noise
Most people are familiar with at least some aspects of these first two strategies and assume they will achieve the desired levels of speech privacy and noise control if they simply provide “sufficient” absorption or build “adequate” walls. This perspective typically goes hand-in-hand with the belief that effective acoustics will only be achieved when the overall volume in the space is as low as possible.
However, just as with other ergonomic factors such as lighting and temperature, there is actually a comfort zone for the volume of sound. This comfort zone can be achieved by controlling the noise floor, which is the level of continuous background sound that characterizes the space. The lower this floor, the easier it is to hear conversations and noises, even those that are relatively low in volume or originate at a great distance from the listener.
Providing a higher and more consistent baseline volume level can easily be accomplished by installing a sound-masking system in the space. This technology is the least known or understood noise control method, though it has been in widespread use for decades, primarily in commercial offices. The FGI Guidelines, Design and Construction of Health Care Facilities and Green Guide for Health Care also recommend its use.
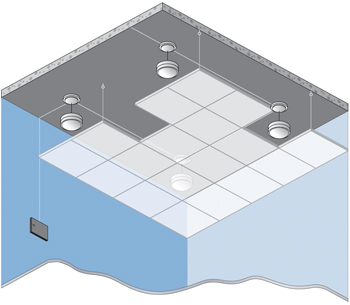
A sound-masking system consists of a series of loudspeakers, which are installed in a grid-like pattern above the ceiling, and a method of controlling both their zoning and output. The sound the loudspeakers distribute is continuous and unobtrusive, maintaining the noise floor at an appropriate volume. When properly implemented, it is highly effective at covering speech. Any noises below the level of the masking sound are also covered up. Furthermore, it diminishes the impact of loud noises by reducing the amount of change between baseline and peak volumes.
The volume to which the sound-masking system is set is well below that shown to decrease sound perception through a stethoscope. Furthermore, because masking requires some distance to become effective, when set to an appropriate volume it will not prevent patients from understanding their caregiver or staff from communicating. In addition, because it is not a physical barrier, it has no impact on caregiver access.
Sound masking has also been found to be a very effective method of improving sleep. Studies show that it shortens the time it takes to fall asleep and helps to reduce sleep disruption due to noise. In fact, in a study of ICU patients, quality of sleep improved by 42.7 percent when sound masking was used.4 Again, the technology’s success lies in its ability to decrease the magnitude of change between baseline and peak volumes. It is this change, rather than the volume of the noise itself, that determines whether or not disruptions or awakenings occur.
It is important to look for a flexible sound-masking system that can provide local control for individual rooms or areas, allowing occupants or staff to adjust the volume as needed. In this case, the masking will not only improve comfort, but also increase patients’ sense of control over their environment. Once installed, a networked system will allow changes to be made without reopening the ceiling, which is key to sanitation. Most sound-masking systems also provide paging and background music functions if needed.
Reduce Noise
One tactic overlooked by the ABC Rule involves the identification and subsequent reduction or elimination of unnecessary sources of noise. Quieter mechanical equipment, hand towel dispensers, and door hardware, as well as rubber-wheeled carts are important. Duct silencers should be installed. Faulty equipment, such as squeaky carts, should be fixed or replaced. Patients should use headphones when watching television. Staff should lower the ringer volume on telephones, turn off unwatched television sets, try to respond to alarms promptly, and be trained to handle loud vocalization by patients.
It is also important to raise staff’s awareness of their own actions, such as talking loudly or yelling down the hallway at each other. Some health care facilities have asked staff to form a special committee to raise awareness of this issue and to develop and enforce policies aimed at controlling noise. Visitors should also be educated about the negative effects of noise and encouraged to follow the rules.
While behavioral changes are necessary, people will always create noise as they go about their tasks. After best efforts have been made to reduce noise at its source, all remaining noises have to be controlled through design using the ABC Rule. A combination of all methods is required because each one plays a unique role in the outcome.
Niklas Moeller is vice president of K.R. Moeller Associates Ltd., a global developer and manufacturer of sound-masking system, LogiSon Acoustic Network. K.R. Moeller is headquartered in Burlington, Ont. He can be reached at nmoeller@logison.com. Also visit www.logison.com
Footnotes:
1. Noise levels and noise sources in acute care hospital wards. D.J. MacKenzie, BSc (Hons) MSc MIOA and L. Galbrun, MEng, MSc, PhD, MIOA, School of the Built Environment, Heriot-Watt University, Edinburgh.
2. Noise and Its Effects. Dr. Alice H. Suter, Conference Consultant, Administrative Conference of the United States (November 1991).
3. Sound Advice – Helpful Information from Stewart Acoustical Consultants. A member firm of the National Council of Acoustical Consultants. 7406 L Chapel Hill Road, Raleigh, N.C. 27607 www.sacnc.com.
4. Stanchina, M.L.; Abu-Hijleh, M.; Chaudhry, B.K.; Carlisle, C.C.; Millman R.P. Pulmonary/Critical Care and Sleep Medicine Division, Rhode Island Hospital and Brown Medical School, 593 Eddy St. APC 7, Providence, R.I. 02903. mstanchina@lifespan.org. Published in Sleep Med. 2005 Sept. 6(5):423-8. Epub 2005, March 31.
